You walked away from treatment, not because you didn’t care, but because it felt too much.
Maybe you missed a session, then another, and then the whole thing slipped away before you even realized it. You didn’t plan to ghost your intensive outpatient program — it just happened.
Now you’re here, asking yourself a question full of fear and curiosity:
“Can this still work for me even if I quit before?”
Here’s the truth before we go any further:
Yes — it can.
And more importantly, the fact that you’re questioning it means you haven’t given up. You’re still open to change. That alone is enough to begin again.
Let’s walk through how you can know — really know — if an intensive outpatient program can still work even after you dropped out.
Your Dropout Was Not a Door Slamming Shut
First, let’s get one thing clear: leaving treatment doesn’t mean the door is closed forever.
In fact, many people who eventually get well don’t stay in treatment the first time they try it. Some leave, pause, get overwhelmed, or shut down emotionally. Some have real‑life pressures that pull them away — bills, kids, jobs, panic.
Dropping out didn’t prove that IOP doesn’t work for you.
It proved that the way it was working before didn’t fit your experience.
That doesn’t mean it won’t work at all. It means it needs to work differently for you.
Understand What “Worked” Even If You Left
Here’s the part most people miss:
Even if you walked away, something worked.
Think back:
- A session that resonated with you?
- A phrase from a counselor that stuck?
- A moment where you recognized a pattern?
These are breadcrumbs of progress — even if they didn’t feel enough at the time.
What didn’t work was likely the pace, intensity, timing, or support structure — not the concept of recovery itself.
That’s important to know, because it means there’s still value waiting to be uncovered.
You Can Return With Intent — Not Obligation
One of the heaviest things about returning to treatment is the fear of being judged.
“Will they think I wasted their time?”
“Will they treat me differently?”
Here’s what you should know:
Programs that understand human beings know this story is common. We don’t see relapse or dropout as “failure.” We see it as data.
You now have real experience — experience that can guide a smarter, more sustainable return.
A good IOP won’t make you start over from zero. They’ll help you restart with intention.
Ask yourself:
- What overwhelmed me last time?
- What would make this approach feel more supportive?
- What do I actually want from this experience now?
Once you answer those questions honestly, you can communicate them clearly to your treatment team.
The Right Intensive Outpatient Program Can Be Tailored
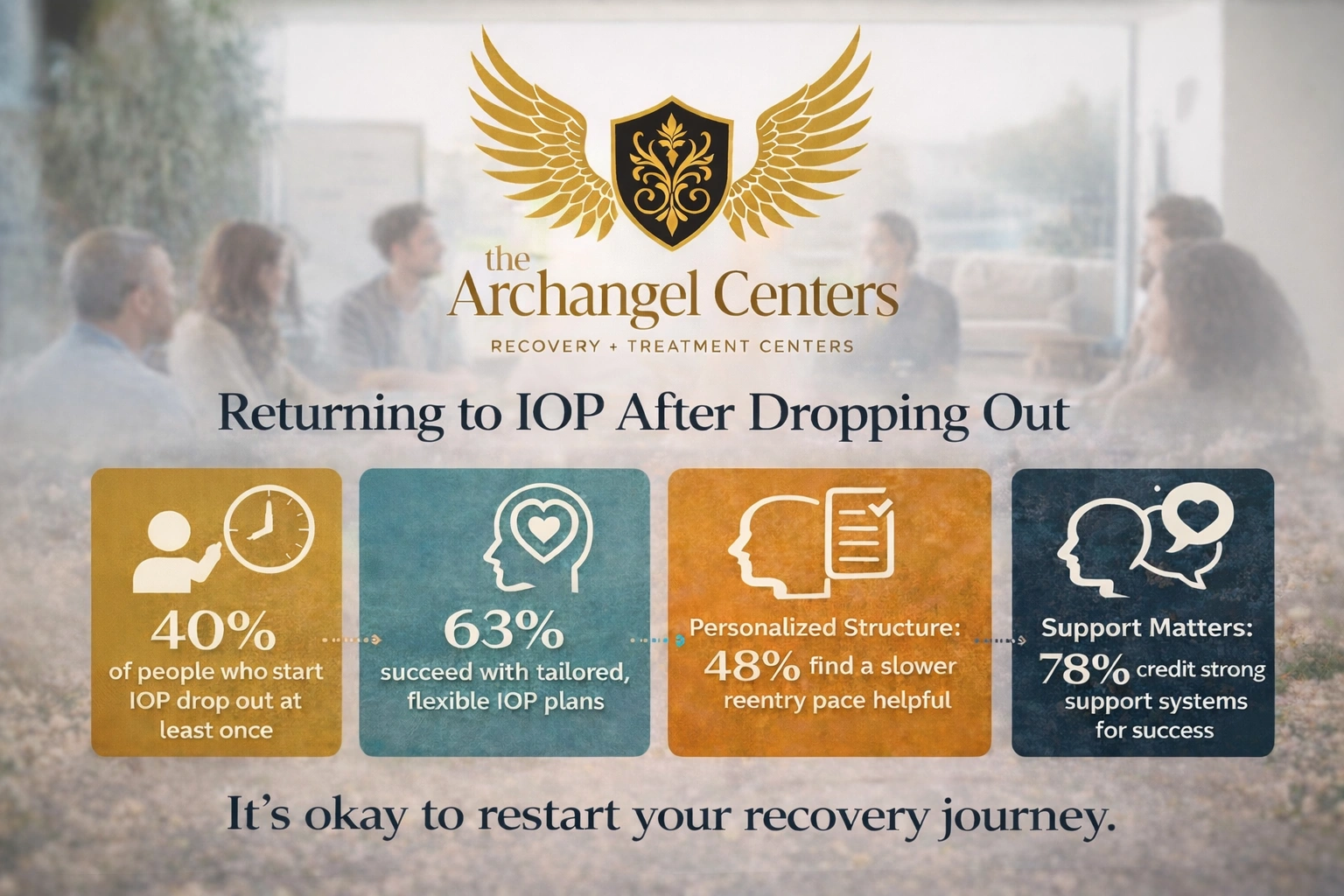
A one‑size‑fits‑all approach rarely works — especially for people who’ve already tried and paused.
Fortunately, good programs understand this and offer flexibility. You can ask for:
- A slower re‑entry pace
- More one‑on‑one time
- Smaller group settings
- A different mix of individual vs. group therapy
- Check‑ins around stress, overwhelm, or triggers
- A plan that acknowledges the previous attempt
This isn’t about making treatment “easy.” It’s about making it workable.
And when it’s workable — when it fits your nervous system — that’s when real change begins.
What Actually Makes IOP Work for People Who Returned
A powerful thing you bring to this second attempt is self‑awareness.
Now you know some of the barriers that knocked you off track before.
That’s a huge advantage.
Here’s what helps people succeed the second time:
Clear Communication About Overwhelm
Instead of silently slipping away when it gets hard, returning clients learn to name the discomfort early.
A Personalized Plan
No two people have the same story. A structured IOP that adjusts to your needs — not just a schedule — makes all the difference.
Support Beyond Sessions
Recovery isn’t only about what happens in the room. It’s about what happens every time you walk out the door.
Tools like text check‑ins, caregiver support, homework grounding practices, reflection journals, or brief daily intentions can help bridge the gap between therapy and life.
Internal Motivation Coupled With Support
This isn’t about being strong. It’s about being supported. Motivation + support = sustainability.
It’s Okay If You’re Afraid to Try Again
There’s a real fear that comes with returning to something that once felt like too much. You might think:
- “What if I fail again?”
- “What if it gets overwhelming again?”
- “What if I just walk out again?”
Here’s the gentle truth:
You won’t be sent back into the same experience that overwhelmed you before.
Returning looks different because you look different now.
You have insight you didn’t have before. You can negotiate your care. You can ask for what you need.
That’s growth.
Where You Can Restart With Support
If you’re in New Jersey, there are programs designed specifically to help people restart in a supportive, human way — not a punitive one.
Archangel Centers offers an intensive outpatient program that meets you where you are, especially if your last experience felt like too much the first time.
Our locations in:
…are spaces where people come back again and again — not because they’re weak, but because they are wise enough to try with more understanding than before.
What to Look for in a Program That Can Work for You
Not all intensive outpatient options are equally equipped to support someone returning after dropout.
Look for programs that offer:
1. Individualized Assessment
A tailored intake that talks about your history — including your experience with dropout — rather than ignoring it.
2. Flexibility in Structure
Not rigid scheduling that punishes absence, but a structure that adapts to your life context.
3. Trauma‑Informed Clinicians
Professionals who can hold your overwhelm without judgment and help you understand it.
4. Clear Expectations With Humanity
Rules are important — but they should be communicated with care and not wielded as weapons.
5. A Focus On Progress, Not Perfection
Success isn’t linear. A good program praises effort, honesty, and consistency — not perfection.
Red Flags That Mean It Might Not Be the Right Fit
If you’re considering returning but worried that an IOP might just repeat the same experience, watch for these signs:
- Staff dismiss questions about overwhelm
- Attendance feels like punishment rather than support
- You feel shamed for past absences
- There’s no option for pacing adjustments
- You leave sessions feeling worse about yourself rather than more hopeful
The right program will meet you where you are — not demand that you be someone you weren’t ready to be yet.
Frequently Asked Questions (FAQs)
Will returning to IOP feel like starting over?
Not necessarily. Good programs honor your previous progress and build on it rather than erasing it.
Can I request a different pace or structure?
Yes. You can—and should—advocate for a structure that feels sustainable for you.
Does leaving treatment once mean I can’t succeed?
No. Many people succeed after returning with clarity and support that wasn’t there the first time.
Will clinicians judge me for dropping out?
In a supportive, quality program, no. Your honesty is valued more than your past attendance.
What if I feel overwhelmed again?
A good IOP will help you work through that feeling rather than push you out the door.
How long does it usually take to feel comfortable again?
Comfort grows with consistency and support. Many clients feel steadier within a few weeks — but everyone’s journey is unique.
You’re Not Broken — You’re Becoming
Dropping out didn’t prove you couldn’t do this.
It proved that the version of treatment you had at that time wasn’t right for you.
Now you’re asking better questions.
You’re not running from treatment.
You’re running toward a way of doing it that actually fits you.
That’s not failure.
That’s growth.
You can come back.
You can build trust with care.
And you can make this work — not by forcing yourself into the old mold — but by finding a version of care that honors your real experience.
Call (888) 464-2144 to learn more about our Intensive outpatient program services in New Jersey.