I used to think treatment was for people who had nothing left to lose.
People whose lives had blown up—who hit rock bottom so hard, they bounced.
I didn’t see myself in that story. I had a job. A partner. A car with insurance and a fridge with groceries. I showed up. I got things done.
But inside, I was unraveling. Quietly. Efficiently. Invisibly.
And I almost let it go too far.
The thing that saved me wasn’t a dramatic intervention or a court order. It was an intensive outpatient program—a few hours a week, with real people and real talk. Not the kind of place I thought “someone like me” needed.
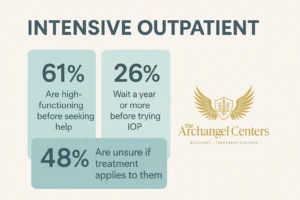
But it turns out, “someone like me” was the exact reason those programs exist.
I Was Fine—Until I Wasn’t
On paper, I had it together. I met deadlines. I texted my mom back. I wasn’t slurring in public or missing rent.
But every night, I drank alone. Not one glass. Several. Not socially. Habitually.
I told myself I deserved it. That I needed it. That it was my “off switch.”
I didn’t miss work. I didn’t black out. So I kept telling myself I wasn’t addicted. That I was managing.
What I wasn’t managing was my energy, my peace, or my shame.
I was doing everything… and feeling nothing. Except tired. Always tired.
The Breaking Point Wasn’t Big—It Was Just Real
It wasn’t a crisis that got me. No accident. No arrest.
It was me, in the kitchen, reaching for a bottle at 10 a.m. on a Sunday.
Not because I needed to party. But because I couldn’t face the day sober.
That’s when the lie I’d been living cracked open.
Because “I’m fine” doesn’t hold up when you need alcohol to get through brushing your teeth.
I didn’t fall apart all at once. I just realized I was already falling.
I Didn’t Want to Lose Everything—So I Asked for Help
Googling “intensive outpatient program near me” felt surreal.
I half-expected the results to be places that didn’t apply to me—locked units, detox centers, rehab in the woods.
But then I found Archangel Centers in Tinton Falls. It felt… different.
I called and said, “I don’t know if I’m bad enough for treatment.”
They said, “If you’re asking, you probably are hurting in ways that deserve care.”
No drama. No pressure. Just clarity.
What I Thought IOP Would Be—And What It Actually Was
I thought I’d have to explain myself.
I thought I’d have to “fit the mold.”
I thought I’d be sitting in a room full of people with wreckage behind them and nothing left to lose.
Instead, I sat next to people who looked like me. Professionals. Parents. College grads. Burned-out humans who were good at pretending.
We talked about things like:
- Drinking in secret
- Feeling like frauds
- Keeping it together by unraveling in private
- Wanting to stop but not wanting to lose control
It wasn’t about labeling ourselves. It was about telling the truth.
Intensive Outpatient Gave Me My Edges Back
IOP wasn’t therapy bootcamp. It was a space to breathe and untangle.
Here’s what it looked like, practically:
- Group therapy 3–5 days a week
- Individual counseling once or twice a week
- Sessions focused on triggers, regulation, self-awareness, and tools—not lectures
- Space to cry, rage, laugh, listen, stay silent, or say the hardest thing out loud
And I still went to work. Still paid bills. Still lived my life.
But now I had tools instead of just a tolerance.
You Don’t Have to Lose Everything to Want More
That’s the myth that kept me stuck the longest:
That if I hadn’t “hit bottom,” I didn’t qualify for help.
But what if your bottom is quiet? What if it’s not a crash—it’s a slow leak?
You’re not weak for catching it early. You’re strong.
You’re allowed to want something better before your life implodes. You’re allowed to be both high-functioning and deeply tired.
IOP didn’t take away my life. It stopped me from losing it while no one was looking.
IOP Wasn’t Easy—But It Was Worth It
There were days I didn’t want to go. Days I rolled my eyes at group. Days I sat in the parking lot wondering what the point was.
But there were also days when I laughed out loud with people who got it. Days I said something that scared me—and no one flinched. Days I walked out feeling lighter.
I got out of it what I put in. And what I put in was my honesty, my fears, and my willingness to try.
What I Gained After IOP
I didn’t get a “perfect recovery.” But I did get:
- Sleep, real sleep
- A less terrified nervous system
- An actual appetite again
- The ability to sit with my thoughts without needing to numb them
- A voice in my head that wasn’t always tearing me down
- Friendships that weren’t built around alcohol
I didn’t lose myself in treatment. I found parts of me I hadn’t seen in years.
If You’re Wondering If You Need Help—That’s the Signal
Not everyone who drinks too much ends up in the hospital.
But many end up exhausted, emotionally flat, and scared to go one night without drinking.
If that’s you… treatment doesn’t mean failure. It means freedom.
Programs like Archangel’s IOP aren’t just for people in crisis. They’re for people who are quietly slipping and don’t want to wait until it’s obvious.
If you’re in Central New Jersey or East Windsor, there are options close to you. The help is real. The judgment isn’t.
FAQs for High-Functioning People Considering IOP
Do I have to quit my job to go to IOP?
No. That’s one of the benefits of intensive outpatient programs. Many clients continue working, parenting, or studying while attending treatment during evenings or flexible daytime hours.
What if I’m not sure I’m “addicted”?
That’s okay. You don’t need a label to deserve support. If alcohol or substances are interfering with your peace, your health, your time, or your self-worth, it’s worth exploring.
Will I be the only high-functioning person in the room?
Absolutely not. Many people in IOP look “fine” from the outside. You’ll meet teachers, nurses, lawyers, college students, parents. Addiction doesn’t always look like rock bottom.
Can I drink sometimes and still be in IOP?
You don’t have to be perfect to begin. IOP will meet you where you are. Some people enter still drinking and taper with support. The point is to build a new relationship with alcohol—whatever that looks like for you.
How long does IOP last?
Typically, 6–12 weeks depending on your needs. Your care plan is personalized. You and your treatment team will decide together when you’re ready to step down or transition to aftercare.
You’re Not Broken. You’re Just Tired. And There’s a Way Out.
Call (888) 464-2144 or visit our Intensive Outpatient Program page to learn more. No shame. No pressure. Just people who’ve been there—and a program that meets you where you are.